Preventing & Managing Delirium
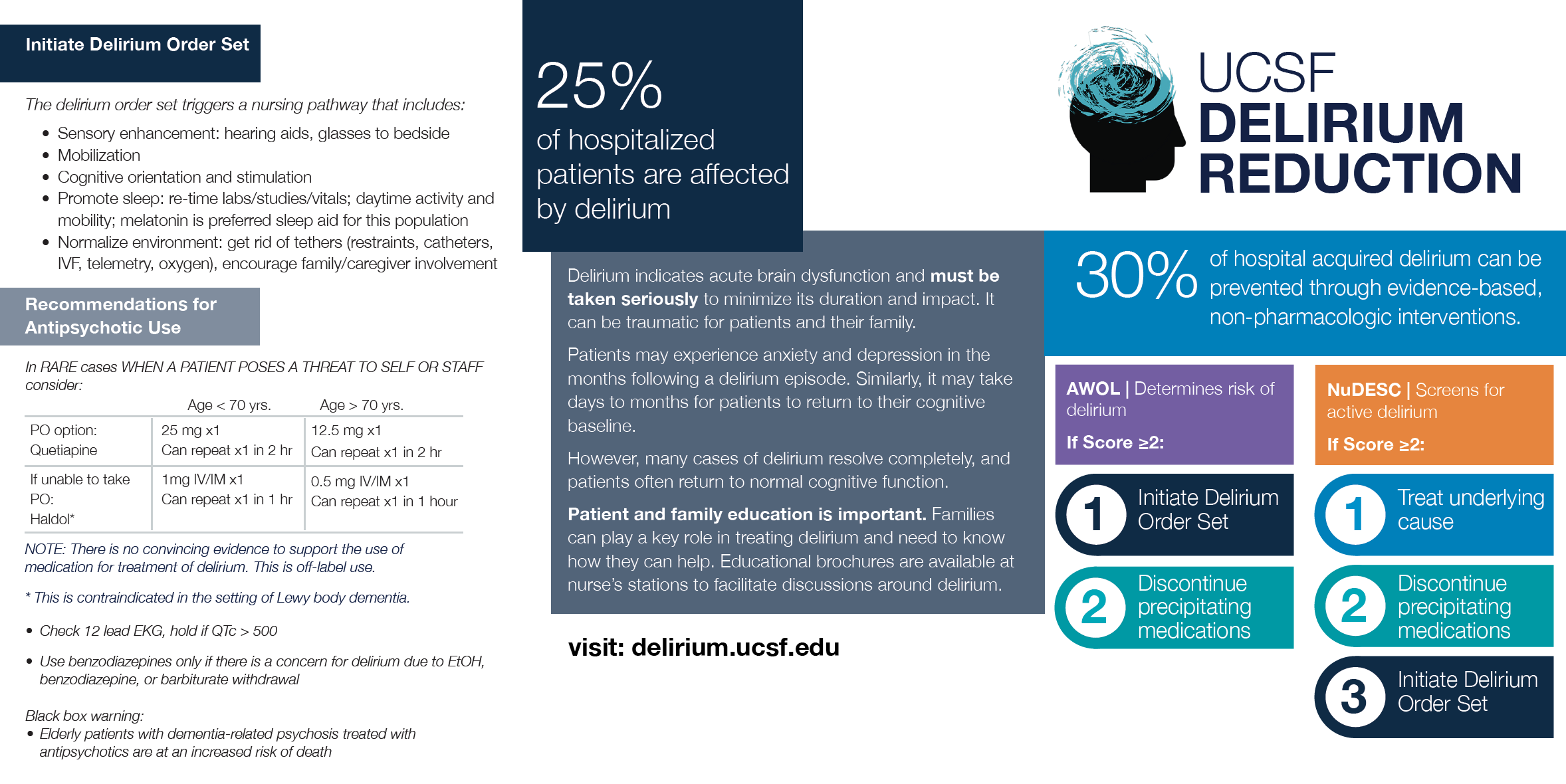
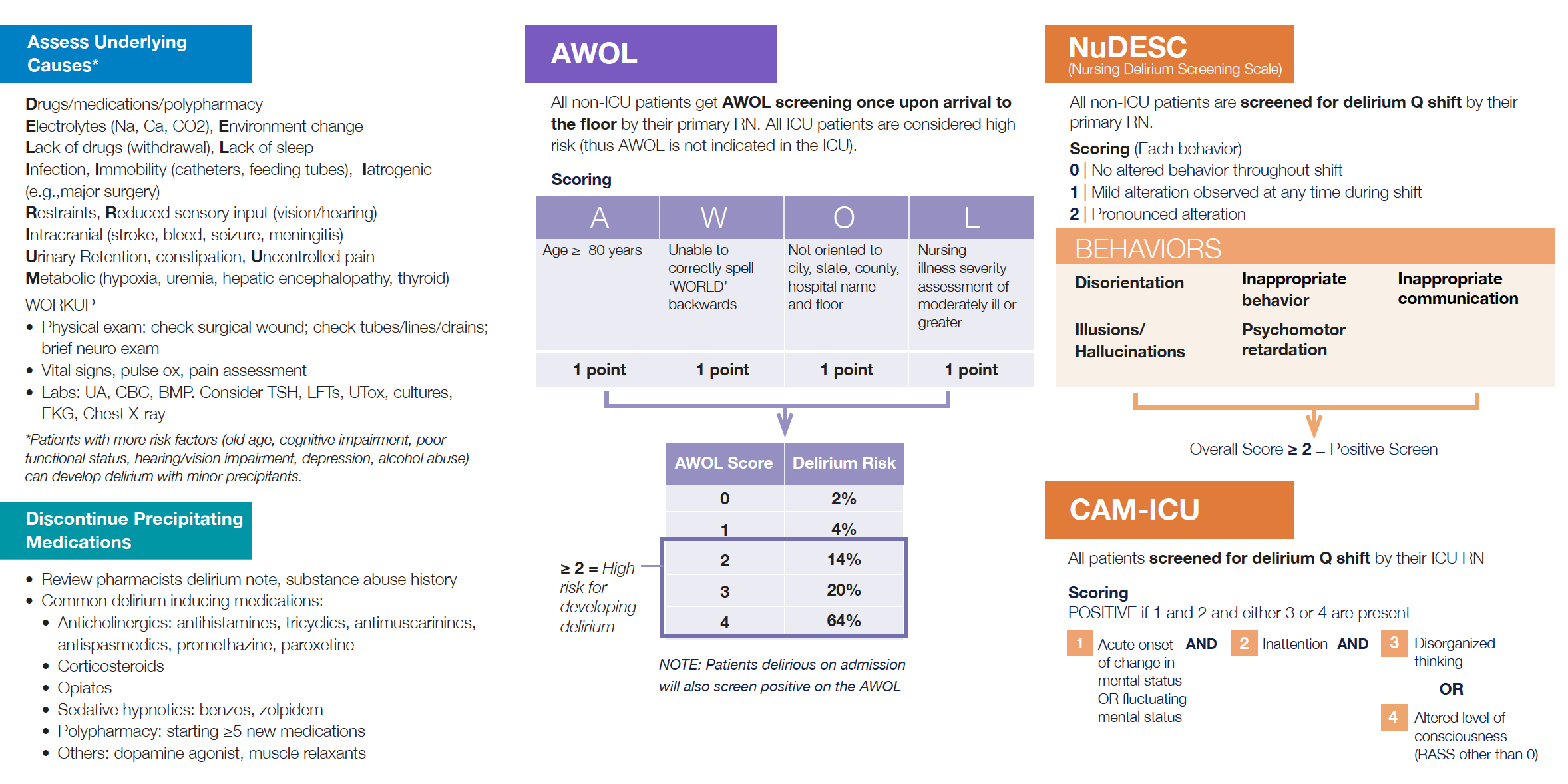
~30% of hospital-acquired delirium can be prevented through evidence-based, non-pharmacologic interventions. A key to preventing delirium is recognizing who is at greatest risk and intervening early to minimize known precipitants to delirium. The AWOL and NuDESC assessments are tools to help you do this. In managing delirium, the most important first step is to identify and correct all potential causes of delirium and avoid any further insults to the brain.
Delirium Management and Prevention Guidelines
RISK FACTORS
- Age (≥80)
- Pre-existing neurocognitive disorders (e.g., DEMENTIA, stroke, Parkinson’s disease)
- Functional impairment (inability to independently perform ADLs)
- Sensory impairment (e.g., hearing and/or vision loss/ impairment)
- Dehydration / Malnutrition
- Depression
- Alcohol abuse
PRECIPITATING INSULTS
D-rugs
E-lectrolytes (Na, Ca, CO2), E-nvironment change
L-ack of drugs (withdrawal), L-ack of sleep
I-ntracranial (stroke, bleed, meningitis) R-estraints, R-educed sensory input (vision/hearing)
I-nfection
U-rinary retention, fecal impaction
M-etabolic (hypoglycemia, uremia, liver failure, thyroid dysfunction, B1 deficiency) / M-yocardial (cardiac bypass)
INTERVENTIONS (as Treatment and Preventation):
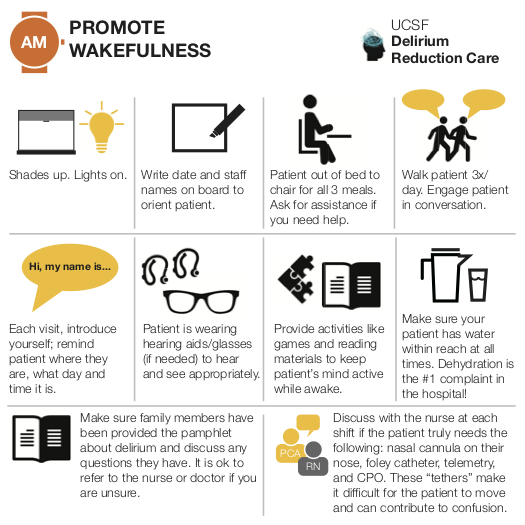
- Promote uninterrupted nighttime sleep and wakefulness during the daytime
- Address cognitive impairment with frequent re-orientation, cognitive stimulation, family engagement
- Minimize sensory deprivation by ensuring glasses and hearing aids are used when patient is awake
- Maximize mobility
- Prevent dehydration, urinary retention, constipation, and uncontrolled pain
AWOL
A score of 2 or higher means patients is at high-risk of delirium and delirium prevention pathway should be implemented
ON ADMISSION, RN needs to:
1. Ask patient 5 orientation questions (city, state, county, hospital, floor)
2. Ask patient to spell WORLD backwards
3. Assess illness severity per RN clinical judgment
SCORING:
1 point each for:
- Age ≥80
- Cannot spell WORLD backwards
- If not fully oriented to: city, state, county, hospital, floor
- Illness severity (RN rates per clinical judgement): moderately ill or worse
In APeX:
- Age auto-populates
- Yes/No dropdown: Is the patient fully oriented to city, state, county, hospital, and floor?
- Yes/No dropdown: Can the patient spell WORLD backwards correctly?
- Illness severity dropdown: not ill, mildly ill, moderately ill, severely ill, moribund
AWOL score auto-calculates and delirium risk is presented:
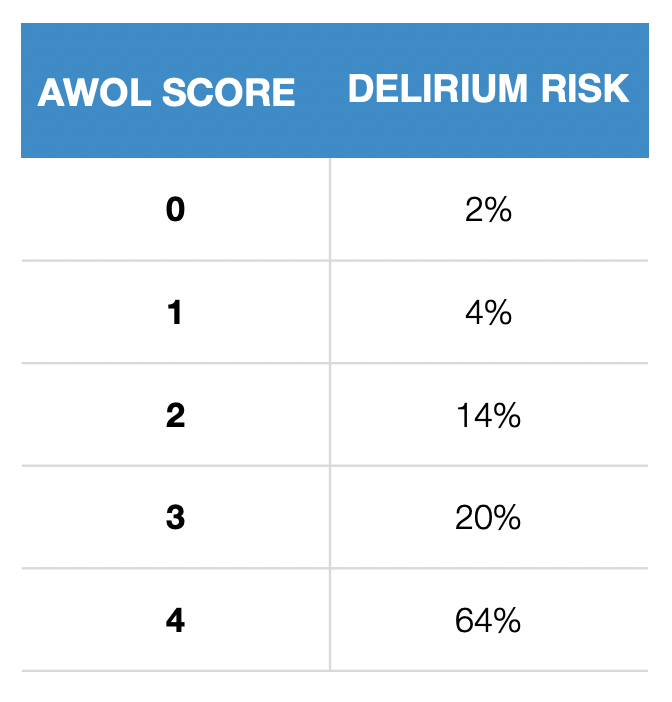
Douglas et al, J Hosp Med 2013
Reviewed 01/2020: Sasha Binford, RN
Nursing Delirium Screening Scale (NuDESC)
1. What is NuDESC
NuDESC is a screening tool that identifies patients who likely have active delirium. Note: it is a screening tool, not a diagnostic tool. A diagnosis of delirium must be made by a physician.
2. Why is it important?
Patients who get delirium are more likely to die within a year, experience hospital-acquired complications (falls, pressure ulcers, and functional decline), stay in the hospital longer, and be discharged to a nursing home. There is also evidence that delirium impacts long-term cognitive health. Moreover, delirium is distressing to patients/families and hard on staff.
Literature shows that without regular, formal screening, nurses and physicians miss delirium 50-75% of the time. Delirium signifies acute brain failure. It is, therefore, imperative that it be recognized promptly so a cause can be identified and corrected as soon as possible.
3. How do I perform NuDESC?
Interact with the patient as you would normally over the course of your shift. The beauty of this screening tool is that it does not require you to do anything additional. Just conduct your standard assessment and note the patient’s behavior and communication.
- Ask open ended questions to determine if your patient can communicate clearly or if s/he seems confused. “Tell me what you understand is the plan for the day.” “What brought you into the hospital?” “How are you feeling?”
- Assess the patient’s orientation to place, time, and situation.
- Note the patient’s level of arousal, response time, and ability to engage.
- Observe the patient’s overall behavior.
4. When do I do it?
Unlike other daily screens (STRATIFY Falls Risk, Braden Skin Scale), NuDESC is intended to be done toward THE END of the shift, as it assesses whether certain behaviors occurred at any point during your time with the patient, as well as the severity of those behaviors. If you suspect delirium earlier in the shift, perform and document NuDESC in that moment.
5. Where do I document it?
NuDESC can be found under Flowsheets → Vital Signs → Nursing Delirium Screening (after the pain assessment).
6. How is it scored?
Toward the end of the shift or with any change in patient’s behavior. We suggest ~4 o’clock when you are documenting vitals to think back on your time with the patient. Each of the 5 items is scored 0-2:
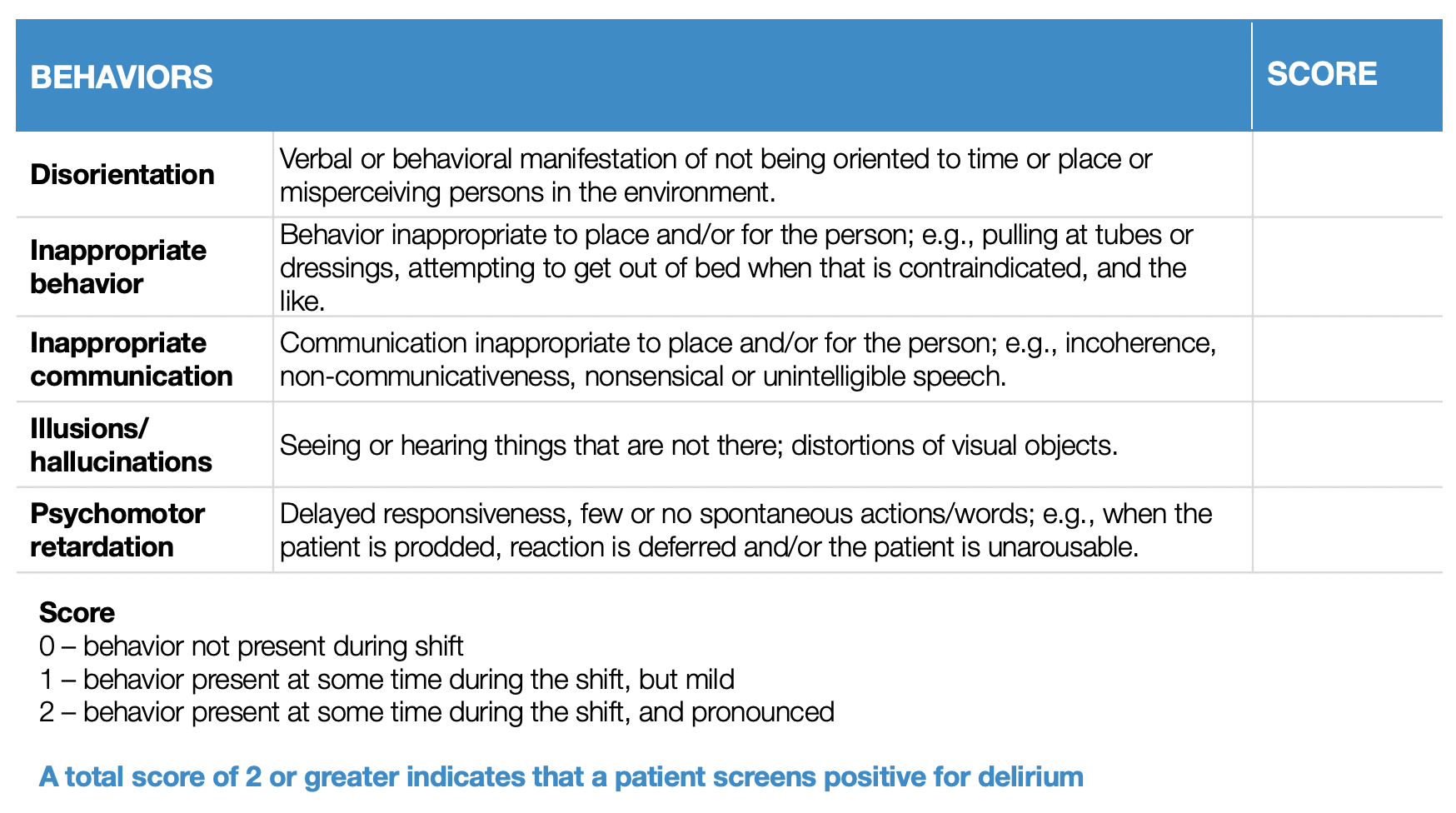
7. What do I do if my patient screens positive for delirium?
The first time the patient screens positive for delirium or if there is an increase from established baseline:
- Notify the primary team and ask them to order the Delirium Order Set and evaluate and correct potential causes of delirium (e.g., infection, pain, reduced sensory input, impaired sleep, urinary retention, fecal impaction, medications). The pharmacist will independently review the medication list for deliriogenic meds and write a note in APeX with recommendations to the primary team.
- Initiate and individualize a Delirium Care Plan. Work with the PCA and rehab staff to execute the interventions.
- Communicate delirium status and care during all handoffs.
8. What if my patient has cognitive deficits at baseline that cause him/her to repeatedly score 2 or greater?
Patients with baseline cognitive deficits, such as those with dementia, h/o stroke, developmental delay, or seizure disorders, may consistently score 2 or greater, but may not have delirium. These individuals are at very high risk of developing delirium, though, so should receive the delirium order set and care plan. The primary team should still evaluate the patient to confirm that s/he is at their baseline.
In the example of a patient with dementia who scores a 2 each shift, if this patient were to then score a 4, it is likely that this patient has delirium on top of dementia and the primary team should be notified to evaluate immediately.
Visual Aids
3"x5" NuDESC scoring aid
Instructions for print production:
- Download the print readh pdf file (click link above) Send to Judy Flannery in Media Services with the following specifications
- Print 1 side full color bleed 80# text; trim to 3"x5" laminate
- Specify quantity you want printed.
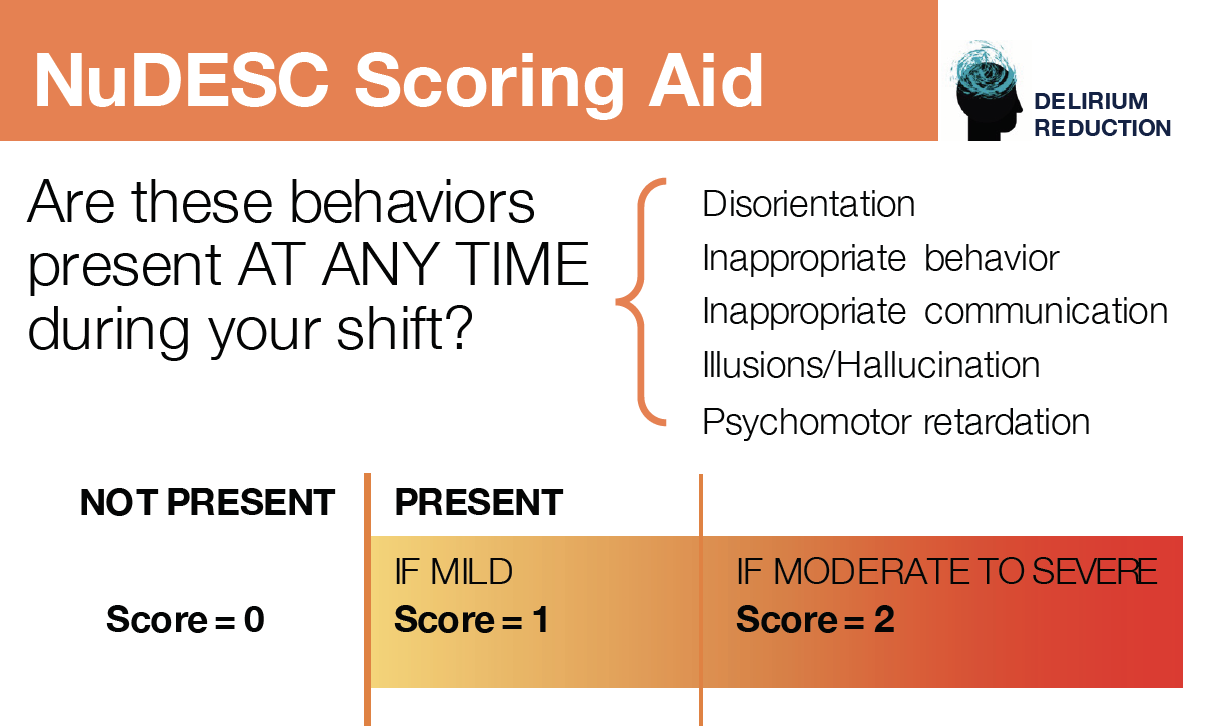
Printing specifications
80# white matte text, 4 color 2 side, print head to head trim to 3.5 x 3.5, 5 mil laminate with lip and slot punch at top
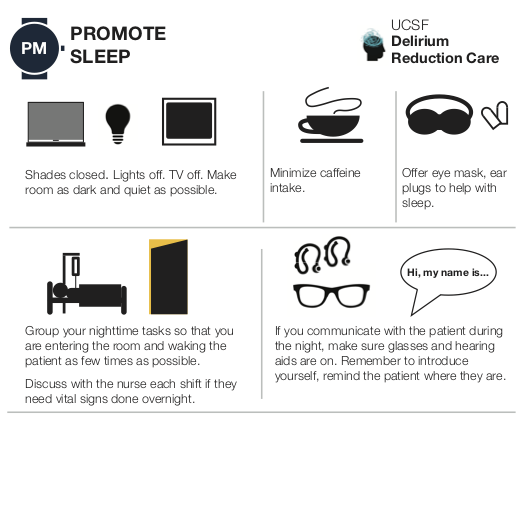
Printing specifications
100# white gloss cover, 4 color, 2/side, use 13" x 19" stock, Trim to 12" x 6", score and fold to 4" x 6"